
This is the second of two stories on the future of the territory’s hospitals. Click here for Part 1 – Struggles of a Public Hospital.
A Delicate Balance
Over the nearly four years since two Category 5 hurricanes swept across the territory, turning many structures into rubble, the hospitals on St. Thomas and St. Croix have been able to offer medical services through sheer will and federal support coupled with a commitment by local engineer Darryl Smalls and his team.
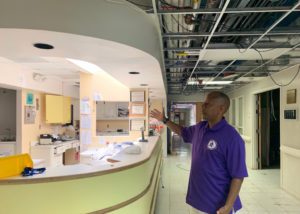
“We’re in a holding pattern,” said Smalls, executive director of facilities and capital development. He used the term “fragile state,” to describe where the hospitals stand figuratively as well as literally.
However, he said, “I see light at the end of the tunnel.”
The flicker Smalls said he sees is the final word from the Federal Emergency Management Agency that the structures Smalls oversees have sustained damages greater than 50 percent. That is FEMA-speak that translates to Smalls being able to move forward with either total or partial reconstruction for the public facilities on all three major islands.
The delays, Smalls said, are normal and though “the process may appear slow,” he said there’s no point in “blaming FEMA.” He said along with the “due diligence” required to ensure that “federal funds are allotted and expended correctly,” the territory is faced with higher construction costs in general – 20-30 percent. Add to that the backlog in production that came with the COVID pandemic and that is a perfect recipe for a slowdown.
Add to that the management required to oversee the process as was outlined in a March joint hospital board meeting and the need for patience seems obvious, if frustrating.
He does see light at the end of the tunnel, however, and is prepared to move into the light soon.
Smalls is ready to go with what he called “selective reconstruction” as soon as FEMA gives the final “go,” which should happen very soon. He said the facilities do not need to be demolished, but do need total renovation, keeping in mind the ways in which health care has changed since they were built.
“We don’t need a 250-bed facility,” he said. “The statistics don’t support it; health care has changed to shorter stays and preventative measures that keep you from coming to the hospital in the first place.”
Nowadays, Smalls said, “Only the most acute cases have to stay.”
But what Smalls believes the USVI does need is skilled nursing inpatient facilities – known as SNIFs, for “wraparound services” for senior assisted living and behavioral health. “That’s where we’re headed,” Smalls said.

Both Smalls and Schneider Regional Medical Center interim CEO Dr. Luis Amaro remarked about the considerations needed when trying to compete with the shiny new private facilities sprouting up around them with their attendant tax breaks and privately insured clientele.
“We’d love to have the Taj Mahal,” Smalls said, adding the newness that will result from the reconstruction will be refreshing. But the bigger challenge faced by the leaders of these facilities is “do we have the staff, and revenue to maintain them,” Smalls said.
“We are charged with making sure we can provide quality care to all patients who walk through the doors.”
“It’s a delicate balance.”


